At Pacific Pain Medicine Consultants, our team has specialized in diagnosing and treating complex pain conditions since 1984. As the first single-specialty pain surgery center in California, our providers combine decades of experience in anesthesiology, physical medicine, and rehabilitation to deliver precision-based, minimally invasive care.
What Is Osteoarthritis?
Osteoarthritis, sometimes called degenerative joint disease, occurs when the cartilage that cushions the ends of bones wears down over time. This breakdown causes bones to rub against one another, leading to stiffness, swelling, and pain. The condition is most common in the hips, knees, and lower back, but can affect almost any joint.
Common causes include:
- Aging: Natural wear and tear over time.
- Injury: Joint trauma can accelerate cartilage loss.
- Obesity: Extra weight increases stress on weight-bearing joints.
- Repetitive use: Overuse of joints contributes to early degeneration.
Osteoarthritis pain tends to worsen with movement and improve with rest. Treatments typically focus on improving mobility and reducing discomfort through physical therapy, regenerative medicine, or joint injections.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune disease in which the immune system attacks the joint lining (synovium). This leads to inflammation that can damage cartilage and bone over time. Unlike osteoarthritis, RA can affect multiple joints at once and often occurs symmetrically—meaning both sides of the body are affected.
Key symptoms may include:
- Warm, swollen joints: Inflammation causes visible redness and puffiness.
- Fatigue and low energy: The body’s immune response can lead to tiredness and malaise.
- Morning stiffness: Symptoms are often worse after rest.
Because RA is systemic, early diagnosis and treatment are essential to prevent long-term damage. Medications that reduce immune system activity, such as disease-modifying antirheumatic drugs (DMARDs), are often prescribed by rheumatologists.
Key Differences Between Osteoarthritis and Rheumatoid Arthritis
While both conditions cause pain and stiffness, they differ in several important ways:
- Cause: Osteoarthritis results from cartilage breakdown, while RA is driven by immune system inflammation.
- Onset: OA develops gradually with age or wear; RA can develop suddenly at any age.
- Symptoms: OA pain worsens with activity, whereas RA pain is often constant.
- Location: RA affects both sides of the body; OA may affect one joint more than another.
Finding the right diagnosis brings clarity and direction. With accurate information and expert care, patients can begin managing symptoms more effectively and restoring confidence in their mobility.
Personalized Pain Relief with Pacific Pain Medicine Consultants
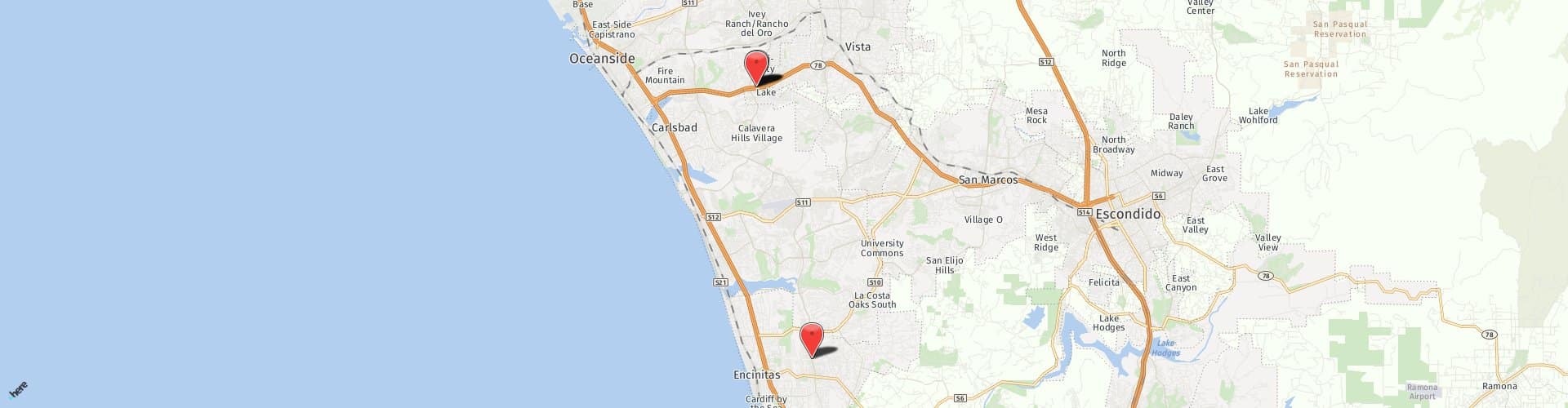
Accurate diagnosis is key to effective arthritis management. Call 760-753-1104 (Encinitas, CA) or 760-943-6494 (Oceanside, CA) to schedule an evaluation and learn more about your arthritis care options.